Moving Beyond Static Snapshots
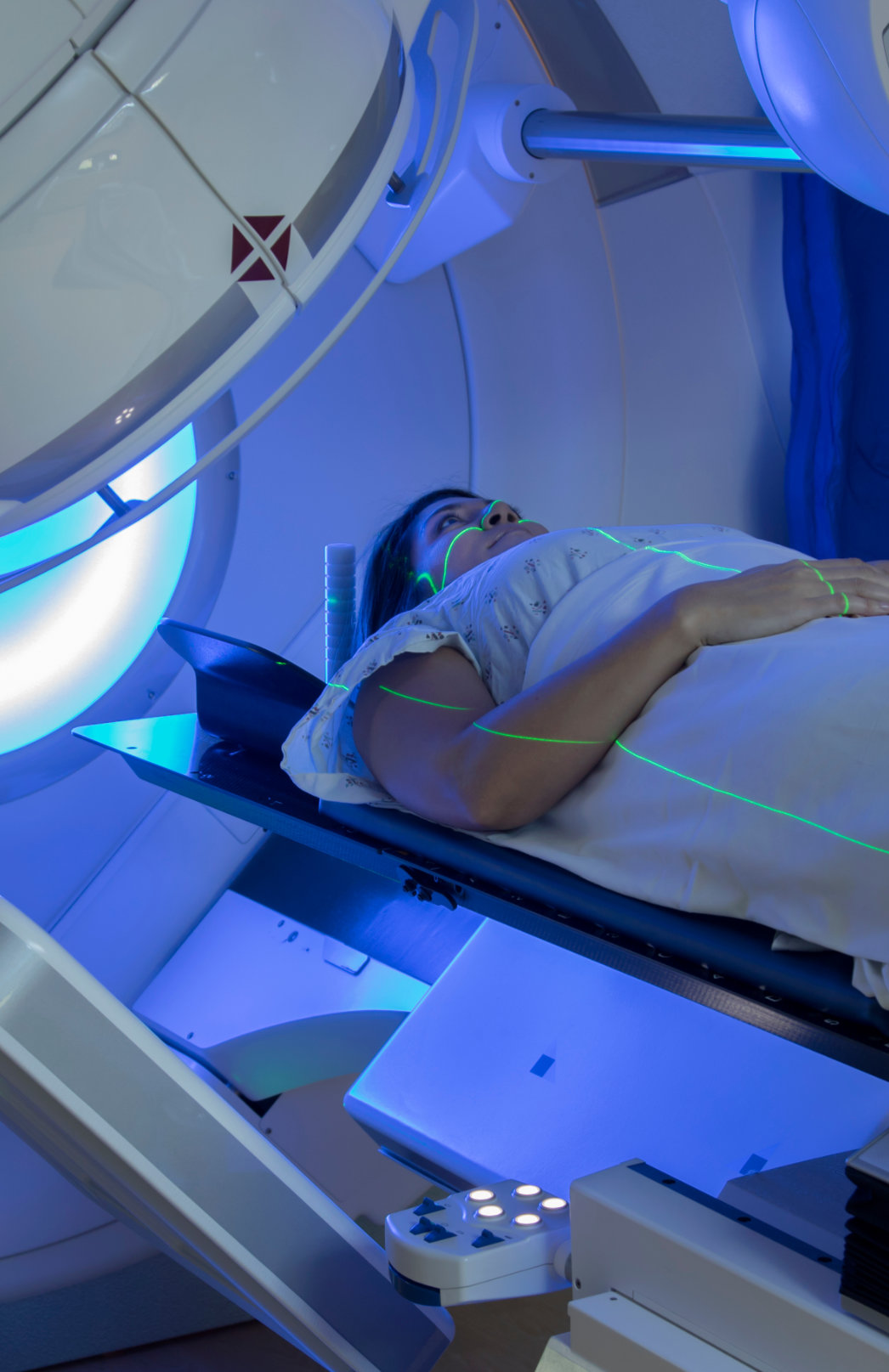
Dynamic Imaging in Adaptive Radiotherapy
Continuous imaging is the foundation of Adaptive Radiotherapy. Without it, the ability to tailor treatment to the patient’s anatomy and tumor response would not be possible. High-quality and progressive imaging ensures clinicians can accurately target tumors, adapt to changes over time, and minimize exposure to surrounding healthy tissue.
With every advancement—CT, CBCT, and now MRI—imaging has steadily improved our ability to visualize tumors and differentiate them from surrounding soft tissue. These technologies give radiation oncology teams an unparalleled view of treatment targets, ensuring accuracy across modalities. Whether used in brachytherapy or external beam radiotherapy (EBRT), imaging provides the assurance that radiation is being concentrated where it is needed most, while healthy tissue and nearby organs remain safeguarded.
Learn About ImplementationSeeing the Difference
Clearer images mean more accurate targeting. Compare CT, CBCT, and MRI to see the difference.

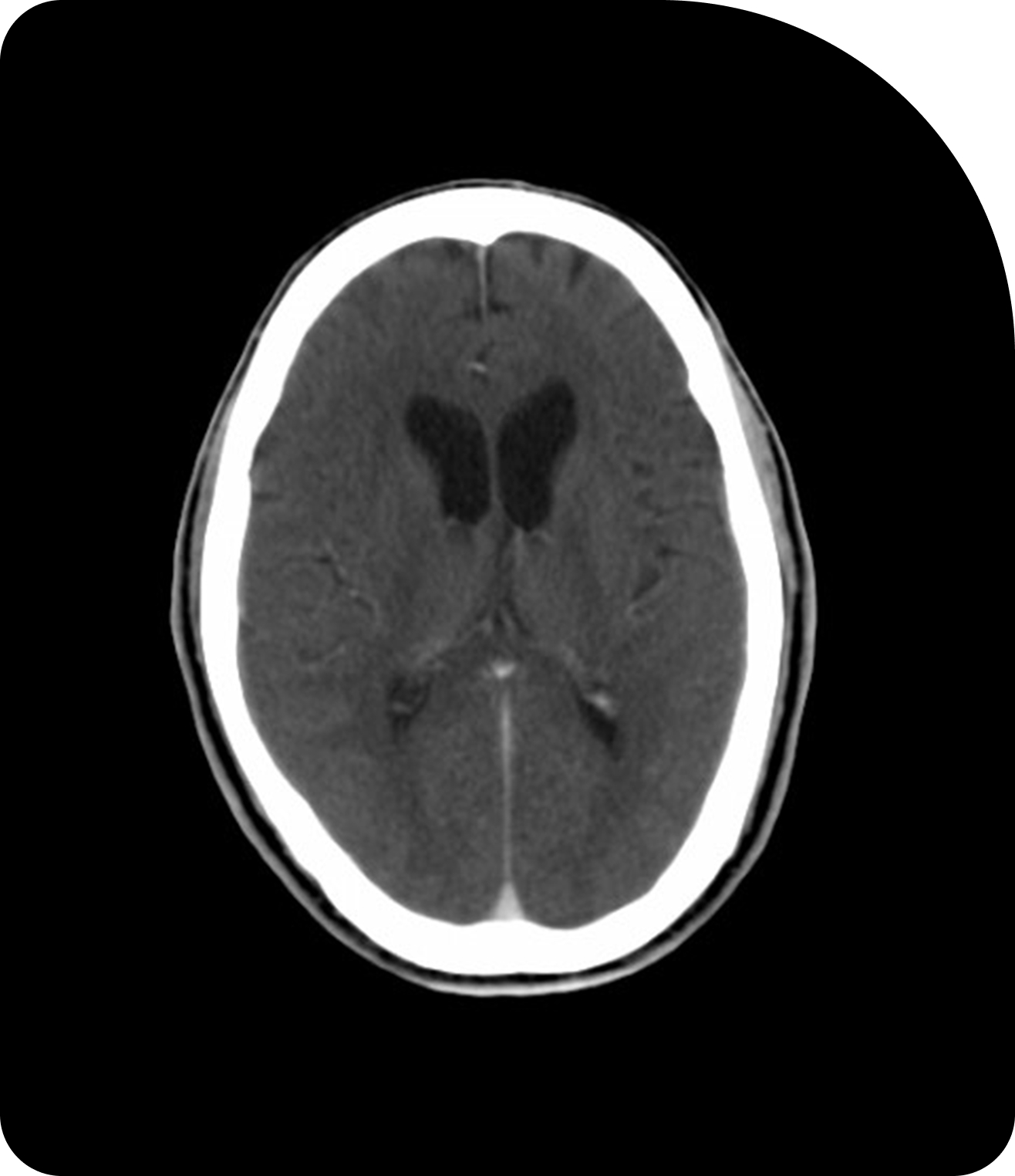
CT
Standard imaging provides a baseline view for treatment planning.
CBCT
Cone Beam CT adds in-room imaging to support daily patient setup.
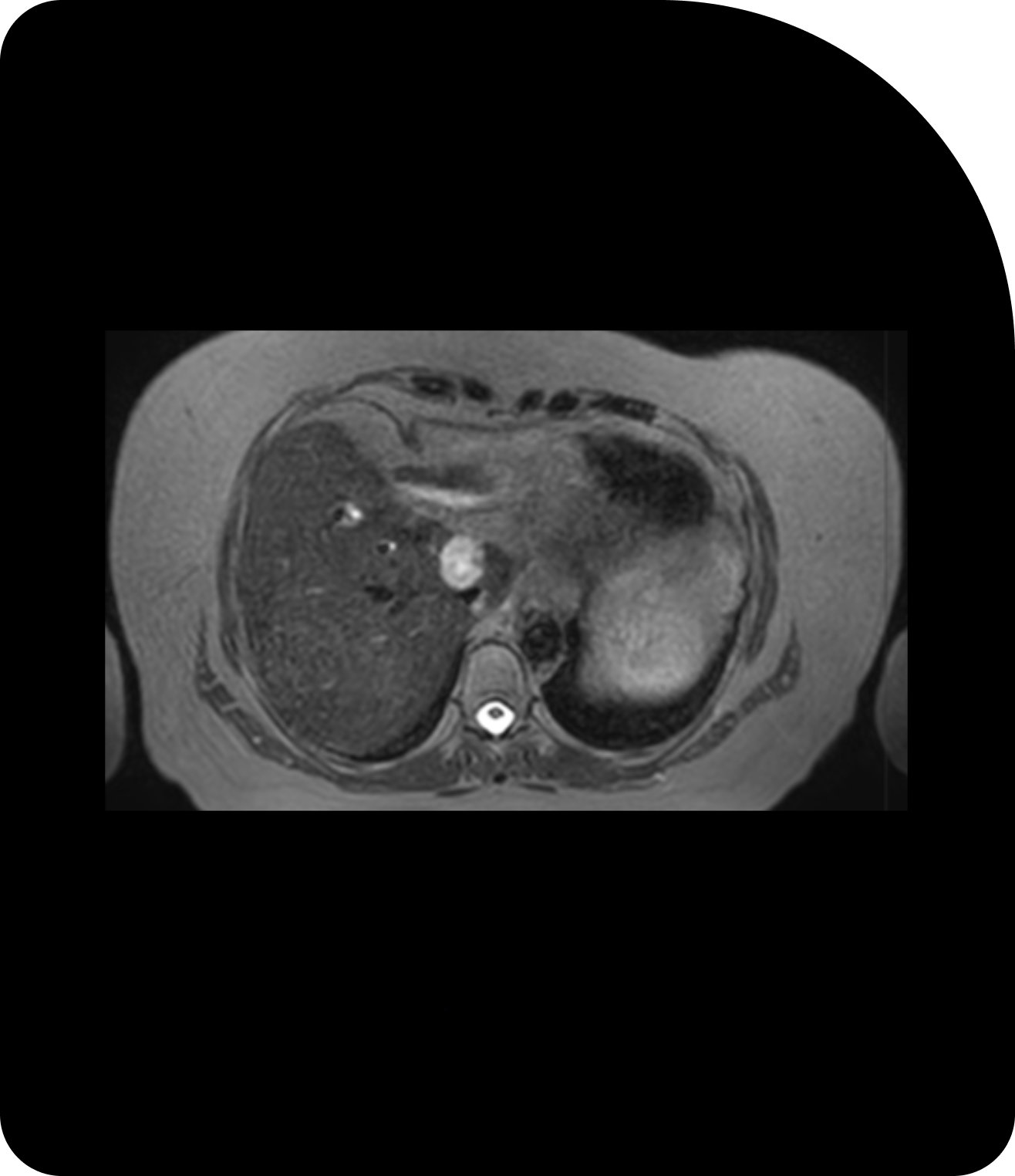
MRI
Superior soft-tissue contrast reveals finer details for precise adaption.
Why Imaging Matters in Adaptive Radiotherapy
Beyond Static Planning
Traditionally, radiation therapy relied on a single planning image taken before the start of treatment. While this provided an accurate assessment of tumor size, shape, and position relative to organs at risk, it did not account for changes that occur over weeks of therapy — such as tumor shrinkage, weight loss, or organ motion — or day-to-day changes resulting from bladder filling, bowel activity, or small changes in the patient’s position on the treatment couch. To account for these changes over time, treatment plans include margins around the tumor that are intended to ensure full coverage. While expanded margins reduce the likelihood of underdosing cancer cells, they typically result in unnecessarily exposing healthy tissue to radiation.
In Adaptive Radiotherapy, imaging is performed more frequently, often daily or even continuously during treatment. This enables clinicians to identify both systematic changes (like gradual tumor shrinkage) and random variations (like breathing or bowel motion) and adapt the plan accordingly. The result is a treatment that is more targeted, safer, and more effective.
Explore ART BenefitsExplore the Research
View Key StudiesModalities that Power Adaptive Radiotherapy
Several imaging technologies enable adaptive workflows, each contributing unique advantages:
Cone-Beam Computed Tomography
Widely used for daily imaging, CBCT provides three-dimensional visualization of the tumor and surrounding anatomy directly on the treatment machine. It helps detect positional shifts and anatomical changes before each session.
MRI-Guided Radiotherapy
MRI delivers unparalleled soft-tissue contrast, making it especially valuable for tumors near critical organs such as the pancreas, or prostate. MRI also enables real-time imaging during treatment, paving the way for innovations like real-time tracking and gating.
CT and PET in Planning
Diagnostic-quality CT and Positron Emission Tomography (PET) scans remain essential for initial treatment planning, offering baseline information about tumor size, location, and metabolic activity. When combined with adaptive workflows, they create a more comprehensive view of disease progression.
Practical Tools
Implications for Clinical Practice
While imaging advances enable unprecedented treatment precision, they also bring new workflow considerations.
Continued evolution of imaging technologies will further enhance the precision of radiotherapy and even enable dose modifications based on the biology of specific cells within a tumor. From initial planning to real-time monitoring, imaging is the foundation that makes Adaptive Radiotherapy possible, bridging the gap between intention and precision in treatment delivery. By harnessing these capabilities, clinicians can deliver therapy that is not only more accurate, but also more responsive to the individual patient, ultimately raising the standard of care in radiation oncology.
Time and Resources
Frequent imaging requires additional time and expertise before and/or during treatment sessions.
Interdisciplinary Coordination
Radiation oncologists, physicists, dosimetrists, and radiation therapists must work closely to interpret imaging, adapt plans, and verify accuracy.
Technology Investment Strategies
Facilities must evaluate whether to implement CBCT-based systems, MRI-guided systems, or hybrid approaches, balancing clinical benefit with cost and operational impact.

